


what
Great
Minds
Can Do
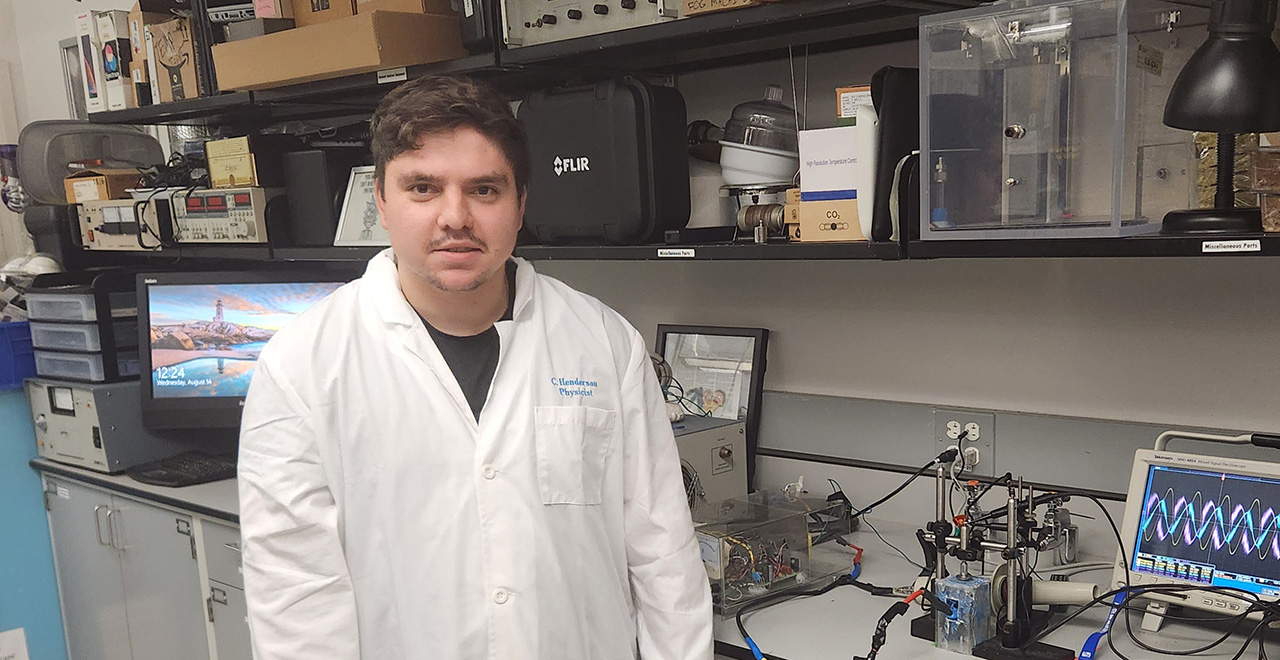
Aspiring physicist and researcher, Christopher Henderson, has teamed up with his professor, Jose Lopez, Ph.D, for a grant-funded study on how plasma can be generated.
Catholic at our core and welcoming to all faiths.
We offer 17k+ professional work experiences.
Best private university in New Jersey for jobs.
An education more affordable than you think.
Diana Malenkova knew she wanted to be a doctor since she was young. She chose Seton Hall because of its rigorous academics and stellar reputation in STEM fields.